In social care, effective communication goes beyond knowledge and expertise to incorporate every aspect of interaction and experience. Care workers need to have the ability to empathise when needed and talk about potentially complicated procedures and issues calmly. Confrontation or disagreements can happen, and the need to defuse these challenging situations is perhaps the most important use of strong communications skills in care. We previously published an article talking about the importance of staff training in health and social care, but perhaps a more important discussion was had in an article about empowerment in health and social care. Written by my colleague Neoma Toersen, her article discusses the risks inherent from clients losing autonomy and feeling like they no longer have control. This is where effective communication comes in, and can help develop a rapport, build a connection, and allow proper discussion about the wants, wishes and needs of the person receiving care. In this article we will assess communication in health and social care, with a particular focus on barriers of communication in health and social care and how we can overcome them – with special mention of our eLearning for care software. Our hope is that by reading this article you will have a better understanding of how to navigate not only the base level of conversation with patients or clients, but also the channels of communication and how to best go about engaging with people to make connections, gain insights, and ultimately improve their care.
Healthcare workers use communication skills (such as those developed by our online communication training) to provide emotional support to patients, protect patient privacy, and to teach new workers how to provide care. The quality of communication in health and social care is crucial because it affects the quality of care that patients receive. Examples of health and social care settings where effective communication is necessary include hospitals, GP surgeries, dentists, nursing homes and social care support centres. When health and social care workers communicate well with each other, and with their patients and their families, patients feel more comfortable and supported. As you probably already know, people should have control over their own care and how it is delivered, in so far as they are able to.
There are many effective methods of communication in health and social care. These include verbal, non-verbal, written and visual communication.
1. Verbal communication This is the most common form of communication and involves communicating through speech. It is important to use clear and concise language when communicating verbally, and to make sure that you are speaking at a pace that the other person can understand. Even this description could be worded simpler to say “keep things jargon free until you know a person’s capability to understand.”
2. Non-verbal communication Body language, facial expressions and physical gestures are all manners of communicating non-verbally. It is important to be aware of your own non-verbal communication, as well as the non-verbal communication of others, in order to effectively communicate. Words only go so far.
3. Written communication Notes, emails, letters and reports. All are written, but while it’s important to use clear and concise language when writing – just as with the speech – it’s more important to use proper grammar and punctuation. Leave no room for error, and if in doubt utilise tools like Grammarly to help.
4. Visual communication Visual communication is things such as charts, graphs and diagrams. If a visuals isn’t easy to understand, it’s not worth using, so factor that in when you’re making a graphic. You are the expert in this case, imparting knowledge. The visual is the short version to hit the key points and help the reader develop an initial understanding.
As you can expect once people enter the care system, they can feel like they’ve lost control of their lives. Simple things they took for granted become harder, day to day tasks might be dictated by a nurse or carer. Good communication in health and social care can avoid the person feeling like this, creating the opening to use their voice more and have their say on their care service.
Person-centred care is a big target within the UK healthcare system. People should always have a say in their own care and how it is delivered if they are able to. Even if your organisation is giving people that control though, poor communication skills can make them think the opposite and undermine your person-focused approach.
Anxiety and depression in care homes is more prevalent than ever before, and a lot of that comes from loneliness. Articles in national papers like the Financial Times and regionals like the Lancashire Evening Post tell stories of loneliness amongst people of all ages, while the BBC even reported on how virtual reality escapism is helping people socialise.
The UK gov website states that “40% of older people living in care homes are affected by depression”, whilst the British Geriatrics Society reported back in 2018 about the increase in depression for care home residents.
Reduced independence in social care is something we’ve also written about here at Access, but it’s more than just that. Isolation, reduced socialisation with family and friends, more medical needs… all of these are stress factors. Proper communication in health and social care settings addresses these and can mitigate a lot of the fear surrounding the change in circumstances.
Good awareness lets carers notice if the characteristics of anxiety issues are present. Does the person feel nervous, are they breathing quicker, are they more irritable? This then feeds into good communication as a way to keep an individual calm. Care worker is as much about the soft skills of talking and engaging with a person as it is checking their health and assisting eating or cleaning. It’s important to engage at the client's pace; let them talk and choose your words carefully to reduce these anxieties and build up their confidence.
One of the barriers to communication in health and social care is money – as it is with most things in life. Money can limit the channels available to communicate with clients, as well as with colleagues. Poor communication as an organisation is as detrimental if not more so than issues with a client.
Poor communication skills can lead to errors such as mistakes on tests and prescribing and administering the wrong medicines. An article from 2014 by The Guardian newspaper cited former UK health secretary Jeremy Hunt and stated that mistakes in the NHS were costing up to £2.5 billion per year – a damning figure that has hopefully been reducing ever since.
Care workers need a select set of skills to be successful when communicating. These develop during their time in care, but must always be present in their role. Some examples include:
Verbal communication
Care workers need to be able to communicate verbally in order to respond to questions, find out about patients' problems or needs, and to draw out all the information they need from a service user as they can come across barriers.
Examples of verbal communication in health and social care include:
Active listening
Active listening is a key communication skill that is taught to health and social care professionals. It is the process of fully attending to another person, using both nonverbal and verbal cues, in order to check understanding of the patient. This requires the healthcare worker to focus entirely on the speaker. Good active listening skills can help to build trust and rapport, resolve conflict, and improve overall communication.
Non-verbal communication
Using non-verbal communication is key. There may be times the service user struggles verbally. Understanding their requirements without the need to be verbal and making sure they understand is important for their care.
Considering cultural differences
Understand cultural differences and how they might impact communication.
These skills may take time to develop as experience and exposure are key, but a carer needs to have natural empathy and be a ‘people person’ - which is something a lot of residents require in their day-to-day lives in care.
Karolina Gerlich, CEO of the Care Worker's Charity, appeared on Access HSC’s ‘Redefining Care’ podcast. Talking to host Anisa Byrne, Ms Gerlich spoke about the skills needed by carers and the lack of recognition. In a blog post on the CWC website, Karoline re-emphasised her point, saying: “Care workers possess an array of skills, including essential “soft skills” like patience, compassion, and kindness, which are unfortunately undervalued. These qualities are intrinsic to individuals and can’t be easily taught or learned unless ingrained during upbringing.”
At Access, we can help your care organisation develop these skills. Our own eLearning for care software provides care professionals with flexible but detailed guides and lessons on how to develop the skills needed to provide the best care possible.
Communication goes two ways. Giving and receiving messages requires consideration of both the carer and service user to make it effective.
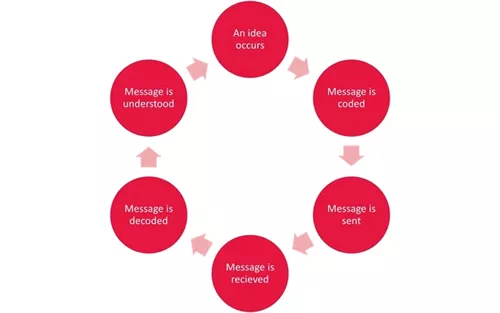
The Cycle of Communication (below) is key to this and is the process of the sending, receiving and decoding of messages. Now, this does not mean you are going to have to start learning Morse Code. The Cycle is totally applicable to the kind of verbal communication that is going on all the time in care, especially with people who may have diminished communication skills, dementia, or difficulty expressing themselves.
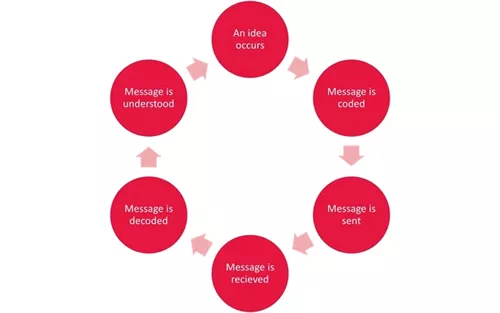
This is where we get a little technical. Argyle’s communication cycle is a theory of effective communication, first developed by Charles Berner in 1965. The simple principle is that the cycle begins when someone, anyone, decides to communicate.
The process involves taking action (message sent), which is then received by the other person (message received). This person then works out the meaning (message decoded) and lets the other person know they have understood (feedback). The feedback is the ultimate response to the initial message and then the whole cycle can start again – if you carry on talking that is!
With communication in health and care it’s important to think about the needs of the service user, since this is the core part of the care worker’s role. Not all service users are the same, so the purpose of the communication must be to establish what the individual requires.
Studies, such as this article from Science Direct have shown that barriers to communication can arise due to a lack of time and staff resourcing, resource scarcity, and increased bureaucracy, making it difficult for healthcare staff to deliver good communication practices. It's important to be aware of these whenever planning, delivering or assessing care.
Below are some of the key barriers to communication in health and social care and how you and your teams can overcome them.
Attitudes, emotion, patience
Our approach and attitude to service users can break down barriers but they can also create barriers. Wherever it is letting frustrations come across to service users, or not treating them in a caring way, it may prevent them telling us how they feel and voicing concerns.
Language barriers
Ensure that any carer visiting a person has the necessary language skills. If the service user’s first language is not English and they don’t speak English well, someone who speaks their native tongue may find communication easier and elicit more detailed, open responses.
Physical and mental health conditions and disabilities
Conditions common in the elderly, such as dementia, Alzheimer’s, or the impact of a stroke, can all affect a person’s ability to communicate their needs and feelings, as well as impacting the thought process. If a person is having trouble communicating, it makes it harder for us to interpret their needs and wants.
Hearing loss is also relatively common in the elderly. Ensuring hearing aids are used where a person has them, or increasing your volume of voice is important. Remember: you may need to speak more slowly, enunciate your words carefully, or perhaps enable a person to use other cues such as reading your lips or body language. If a person is deaf and knows British Sign Language you may also want to learn some basics - it can make a big difference and break down communication barriers whilst building trust and confidence in your skills as a carer.
Learning disabilities can often impact a person’s ability to communicate, in these instances it is essential to identify what ways these difficulties can manifest and what techniques/approaches can be used to make communication more effective.
This is where effective communication becomes vital. By mastering effective, empathetic communication we can help reassure a person who is confused or fearful. By maintaining patience and understanding of how their condition feels, we can reduce distress, enabling them to relax and be more open and honest. By learning more about conditions like dementia we can adopt approaches to help them, or at least communicate their thoughts and feelings more easily.
Other factors
Factors in the home, or care setting can also have an impact. Loud televisions, poor lighting, background noise, distractions, and even face masks can all impact our ability to communicate effectively in care. Even if a person is uncomfortable (too warm or cold, for example) they may be distracted and less communicative as a result.
Barriers to communication in care can reduce the quality of the care service for people and make them less open and honest. In turn this can be reflected in your inspection by regulatory bodies.
More importantly, barriers to communication can also mean we miss out on opportunities to notice deterioration of a person’s health and wellbeing, or to improve the care service for the person, in little or big ways, all of which can make a significant difference to care quality.
Why is clear speech important in health and social care?
If a person feels they can’t hear or communicate – or worse they are not being listened to – it can further a sense of disempowerment that we don’t want to see in people who may have already lost a significant amount of autonomy. Open, honest, communicative, listening care is a better service.
You can’t avoid barriers of communication in health and social care, but you can work around them or remove the obstructions.
Although a lot of these barriers are transferable between conditions, preparation is the key to success. Care workers need to be ready for any problems that may arise with poor communication, so they can deal with it effectively and in the best way for the resident.
The best way to prepare is to learn, and keep on learning. Learn from this article, or from our soft skills communication course. Learn from experts in care and clinicians elsewhere in healthcare. Be open to new information and changing your own habits and attitudes. You might not notice it at first, but you will grow as a person, and it is this growth that will make you a better carer.
If you found this article helpful then why not consider our Learning and Development Guide, covering the top 7 challenges in learning and development for care providers and how to overcome them.